High Eye Pressure After Cataract Surgery
There is good news and bad news about the pressure in the eyes after cataract removal. The good news is that cataract surgery tends to lower eye pressure once you heal. The bad news is that cataract surgery can raise pressure for the first week or so while you are healing.
High Eye Pressure after Cataract Removal
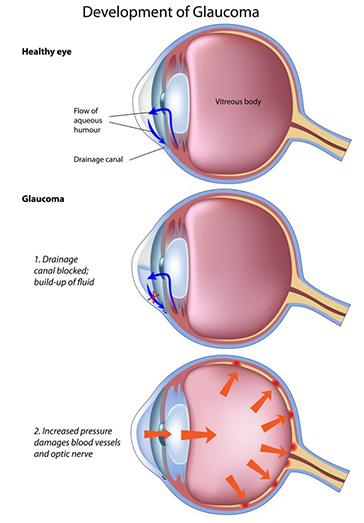
Fluid is being made in your eyes every minute of every day. This fluid escapes the eyes right where your cornea and your iris connect. We call this area “the angle.”
To protect your eyes and keep it formed during the procedure, we place a thick substance inside your eyes called “Viscoelastic.” This viscoelastic is one of the great advances of modern cataract removal. At the end of the procedure, we remove most of the viscoelastic, but some always remains. This slowly dissolves and is absorbed by your eyes.
In addition, your eyes release proteins during surgery. Both the thick fluid from the proteins released and the retained viscoelastic slow how fast fluid leaves the eyes. This can cause pressure in your eye to temporarily go up for the first week or two after your cataract removal procedure.
If eye pressure is just moderately elevated, the eye doctor will notice it the next day at your postop visit. He/she will likely prescribe an eye drop like Timolol, Alphagan, Azopt, Combigan, or Travatan.
Once the thicker fluid is cleared from the eye, the eye pressure returns to normal and the eye pressure drop is stopped.
Complications of Cataract Surgery
If the pressure is dangerously elevated, it will usually cause eyeaches (like a tooth ache) and sometimes it will even make you feel nauseated the evening after your surgery. This is one of the potential complications of cataracts surgery.
If this happens, then it is important you call your expert eye surgeon that night. If the pressure is elevated, eye drops will be started or other techniques employed to lower pressure , make you comfortable, and protect your vision.
After surgery we usually have you take a steroidal anti-inflammatory drop. These are very helpful for most patients in their healing process. However, in a small percentage of patients, they can cause discomfort to go up after using them for several weeks. This is part of the reason we see you for follow up appointments. If your discomfort does rise, the steroid drop is often discontinued and pressure-lowering drops may be started to return your eye to normal.
Lower Eye Pressure After Cataract Surgery Healing
At the last meeting of the American Society of Cataract and Refractive Surgeons (ASCRS) last spring, I was asked to present data on the long term effects of cataract surgery on eye pressure in a Glaucoma/Cataract Symposium.
The good news is that, on average, surgery does lower the discomfort in our eyes once you are fully healed. The higher your pressure before the procedure, the more the discomfort tends to lower.
This is particularly beneficial for those with glaucoma that really need to have lower pressure in your eye for the long-term safety of their eyes.
Microstents to Lower Intraocular Pressure After Cataract Removal Surgery
In recent years, a number of micro stents have been developed to lower pressure in your eye even more than surgery alone. These are inserted into the angle at the time of surgery to increase the flow of fluid out of the eye long term.
The iStent is already FDA approved and does a good job for patients. I am currently in FDA trials for two other products that also aim to help those with glaucoma lower there pressure even further after cataract removal. These are made by Transcend and Glaukos. I will keep you posted on these options as the data from the studies becomes public.
If I can provide any further information about eye pressure and cataract surgery, please leave a comment or contact me at my office.